°
F)
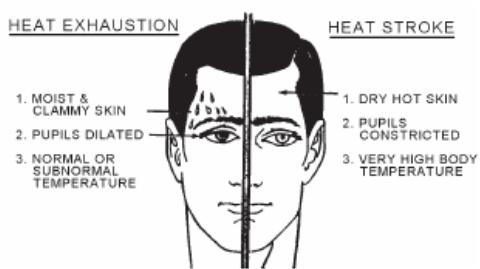
- Dilated pupils
Treatment
- Move to cooler location
- Actively cool casualty by
wetting the head and upper torso with water and fanning
- Salt replacement with sports
drink or IV fluids
- Loosen or remove clothing
- Restriction of activities for the next few days
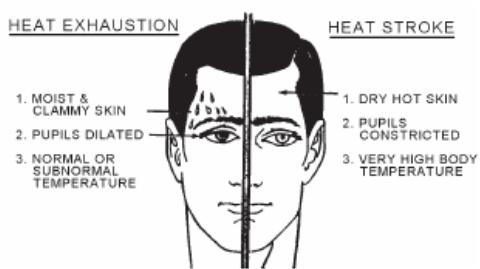
Figure 2. Differences
between Heat Exhaustion and Heat Stroke
|
Heatstroke - severe, life-threatening condition.
A
TRUE MEDICAL EMERGENCY!
Cause - impaired heat loss mechanisms. It is a total
failure of the thermoregulatory mechanism, resulting in an excessive rise in
body temperature.
Signs and Symptoms - the most significant difference
in heat stroke compared with heat exhaustion is neurologic disability which
presents as mental status changes (confused, disoriented, combative, or
unconscious). Other signs and symptoms are:
- Dry, hot, red skin
(rectal temperature usually greater than 106°
F)
- Respirations - deep, then
shallow, then absent
- Pulse - rapid and strong,
then rapid and weak
- Blood Pressure - elevated
initially, then hypotensive
- Dizziness/weakness
- Nausea and vomiting
- Constricted pupils
Treatment
- The
PRIMARY goal and focus should be to reduce the body’s core
temperature.
- Maintain
ABC’s
- Gain IV
Access – give a 500 mL fluid challenge and reassess vital signs. Do not give
more than 2 liters within the first hour. Vigorous fluid resuscitation may
precipitate development of pulmonary edema.
- Monitor
core temperature every 5 to 10 minutes. Active cooling measures should stop
when core temp reaches 102.2° F
- CASEVAC
5.
METHODS OF COOLING THE BODY
Direct Cooling
- Apply ice
bags to vascular areas of the body such as axilla, groin, scalp, and neck
regions.
- Place a sheet over the casualty and wet
the sheet with cool fluid. Fanning the wet sheet while on the casualty will
also quickly reduce the temperature.
Room Temperature Water Misting - fast
method of cooling the body that requires only minimal monitoring of the
casualty.
- Spray or
mist a semi-nude heat casualty on a mesh hammock applying a film of water on the
skin.
- A fan may
also be utilized to increase the effectiveness of this method.
This method does not require cold
or ice water. Room temperature water is all that is required. This method can
also be used to treat multiple casualties simultaneously.
Immersion
- Cooling the body through conduction.
- Immerse
the patient in a bathtub filled with ice water (not usually available in field
environment).
- Requires constant monitoring
of the patient during the procedure.
- This method takes 10-40
minutes.
- Concerns when using ice water
immersion:
- Peripheral vasoconstriction
would impede the rate of heat loss.
- Shivering generates heat and
would increase heat production.
- Hypothermia if the patient is
left in the water too long.
- Difficulty monitoring the
body core temperature.
6. PREVENTIVE
MEASURES OF ALL HEAT INJURIES
Education of Personnel (MOST IMPORTANT PREVENTION MEASURE)
Proper Water Intake
- During
hot weather operations, sweating can cause loss of body water in excess of 1
liter per hour. Personnel must be trained to drink liberal quantities of water.
- Water alone will not prevent an individual from becoming a heat casualty.
Sodium and potassium must be replaced along with water. Personnel must be
trained that an adequate diet (MRE's/Messhall) is essential for proper
water/electrolyte balance. (See lesson on Dehydration Casualties).
Proper Acclimatization
- In some areas this may take
from two to four weeks (3 weeks optimal)
- Gradual introduction of physical training program
Proper Clothing
- When
situation permits, wear the least allowable amount of clothing.
- Avoid
skin exposure to direct sunlight (burned skin is less able to regulate body
temperature).
- Clothing should be loose fitting to permit air circulation, especially at the
neck, arms, waist, and lower legs.
Work Schedules
- Tailor
work schedules to the situation with careful consideration to heat/humidity
index, acclimatization time, type of work and place.
7. HEAT CONDITION
FLAG WARNING SYSTEM
Wet Bulb Globe
Temperature (WBGT) Index - a composite temperature used to estimate the
effect of temperature, humidity and solar radiation have on humans. This index
uses the combination of a dry bulb for ambient temperature, wet bulb for
humidity measurement, black globe for radiant heat and air movement to provide a
more accurate impact of the environmental conditions. It is NOT the same as
regular air temperatures. The WBGT can be monitored hourly and the
corresponding colored flag placed on a flagpole outdoors for all personnel to
see. Where appropriate, adjustments of clothing, physical activity, work/rest
cycles, and fluid intake can then be made based on these conditions.
Flag Warning System - color-coded flags are
used to help prevent heat casualties during hot weather. These flags will be
prominently displayed by all commands so that every one can see them,
particularly in areas where physical training takes place.
White Flag (less than 80°
F) - extremely intense physical exertion may precipitate heat exhaustion or
heatstroke. Caution should be taken. (No flag is flown for white flag
conditions).
Green Flag (80°
F to 84.9° F) - heavy exercises for
unacclimatized personnel will be conducted with caution and under constant
supervision.
Yellow Flag (85° F to
87.9° F) - strenuous exercises, such as
marching at standard cadence, will be suspended for unacclimatized troops in
their first 2 or 3 weeks. Outdoor classes in the sun are to be avoided.
Red Flag (88° F to 89.9°
F) - all physical training will be halted for those troops who have not become
thoroughly acclimatized by at least 12 weeks of living and working in the area.
Those troops who are thoroughly acclimatized may carry on limited activity not
to exceed 6 hours per day.
Black Flag (90° F and
above) - all strenuous outdoors-physical activity should be halted for
all troops.
REFERENCES
Naval Preventive Medicine Manual, P5010, Chapter 3
Wilderness Medicine, Pgs 41-44 and Chapter 8
Pre-hospital Trauma Life Support, Military Edition, 6th
Ed, Chapter 16
REV: July 2008
Heat Injuries Review
1.
List the six predisposing (host) factors associated with heat injuries.
2. List
five signs or symptoms of heat exhaustion.
3.
Identify the most significant difference between heat stroke and heat
exhaustion.
4. List and describe the three
methods of cooling a patient suffering from a heat injury.