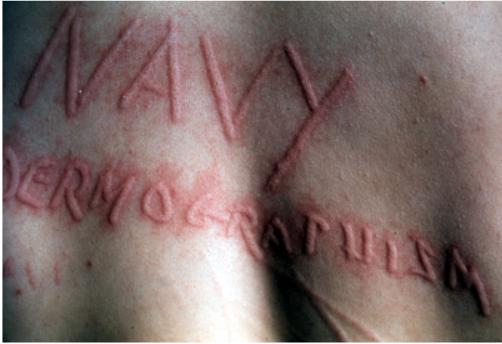
Urticaria and Angioedema
Preface · Administrative Section · Clinical Section
The
General Medical Officer Manual , NAVMEDPUB 5134, January 1, 2000
Bureau
of Medicine and Surgery, Department of the Navy, 2300 E Street NW, Washington, D.C.,
20372-5300
This web version of The General Medical Officer Manual, NAVMEDPUB 5134 is provided by The Brookside Associates Medical Education Division. It contains original contents from the official US Navy version, but has been reformatted for web access and includes advertising and links that were not present in the original version. This web version has not been approved by the Department of the Navy or the Department of Defense. The presence of any advertising on these pages does not constitute an endorsement of that product or service by either the Department of Defense or the Brookside Associates. The Brookside Associates is a private organization, not affiliated with the United States Department of Defense. All material in this version is unclassified. This formatting © 2006 Medical Education Division, Brookside Associates, Ltd. All rights reserved.
Home · Textbooks and Manuals · Videos · Lectures · Distance Learning · Training · Operational Safety · Search
|
|
|
This website is dedicated to the development and dissemination of medical information that may be useful to those who practice Operational Medicine. This website is privately-held and not connected to any governmental agency. The views expressed here are those of the authors, and unless otherwise noted, do not necessarily reflect the views of
the Brookside Associates, Ltd., any governmental or private organizations. All writings, discussions, and publications on this website are unclassified.
© 2006 Medical Education Division, Brookside Associates, Ltd. All rights reserved
Other Brookside Products