1.
Given the requirement in a tactical environment, necessary equipment
and supplies, perform care of the feet, to prevent serious foot
injuries. (FMST-FP-1604)
ENABLING LEARNING OBJECTIVE
1.
Without the aid of references, given a list, identify the types of
foot disorders, per the student handout. (FMST-FP-1604a)
2.
Without the aid of references, given a description or list, identify
the symptoms of foot disorders, per the student handout. (FMST-FP-1604b)
3.
Without the aid of references, given a description or list, identify
the proper treatment for foot disorders, per the student handout.
(FMST-FP-1604c)
4.
Without the aid of references, given a list, identify preventive
measures for foot disorders, per the student handout. (FMST-FP-1604d)
1.
ANATOMY OF THE FOOT
 |
Side view of the right foot. |
 |
Top view of the right foot. |
 |
Front view of superficial muscles that move the foot
and toes. |
 |
Top side view of superfacial muscles that move
foot/toes. |
 |
Back view of superficial muscles that move the foot and
toes. |
 |
Back view of deep muscles that move the foot and toes.
|
Substitute
Figure 1. Anatomy of the foot*
2.
COMMON TYPES FOOT DISORDERS
Blister
- A blister is a
defense mechanism of the body. When the epidermis layer of the skin separates
from the dermis, a pool of fluid collects between these layers while the skin
re-grows from underneath. Blisters can be caused by chemical or physical
injury. An example of chemical injury would be an allergic reaction. Physical
injury can be caused by heat, frostbite, or friction.
Causes
- Improperly
conditioned feet
- Heat and
moisture
- Improperly
fitting boots and/or socks
- Friction and pressure
Signs and
Symptoms
- Fluid collection under the skin
- Mild edema
and erythema around the site
- Sloughing of
tissue exposing subdermal tissue layer
- Localized discomfort and/or pain
Treatment
Small blisters usually need no treatment
- Clean area with soap and water
- Monitor for signs and symptoms of infection
- Apply a protective barrier (moleskin bandage) around the blister, to prevent
further irritation
Closed, Large blisters (if affecting individuals gait)
- Wash the area around the blister with Betadine solution or alcohol pad
- Drain as close to the edge of the blister as possible to allow for drainage,
and then apply gentle pressure to the blister dome expelling the clear fluid
- Apply moleskin (donut) to skin surrounding the blister, using tincture of
benzoin as an adhesive.
- DO NOT PUT ANY ADHESIVE DIRECTLY ON THE BLISTER
- Dust entire foot with foot powder to lessen friction and prevent adhesive from
adhering to the socks
- Monitor for signs and symptoms of infection
Open
blisters
- Wash with Betadine solution or clean with soap and water
- Remove any loose skin with a surgical blade or scissors
- Apply moleskin (donut) to cover skin surrounding the blister, using tincture
of benzoin as an adhesive.
- Place a small amount of antibiotic
ointment over wound
- Cut a telfa pad and place it inside the moleskin
- Apply moleskin over entire treated area to include surrounding skin
- Monitor for signs and symptoms of infection
Athletes Foot (Tinea Pedis) - Tinea pedis is a chronic fungal
infection of the feet, often referred to as athlete’s foot. Athlete’s foot is
very common and usually begins in early adulthood. Men are more often affected
than women. Once affected, recurrences are common.
Causes
- Hot humid weather, excessive sweating, and occlusive footwear
- Contact with contaminated footwear and floors
- Poor foot hygiene
Signs and Symptoms
- Itching,
burning and stinging sensation usually between the toes
- Sore, purulent, weeping rash
Treatment
- Apply anti-fungal foot powder daily during work hours – i.e. Miconazole
- Apply anti-fungal ointment daily during rest hours – i.e. Clotrimazole
- Treatment should be continued for 1 week after clearing has occurred
- If the patient fails to respond to treatment, refer patient to Medical Officer

Substitute Figure 2. Infected Ingrown
Toenail* |
Ingrown Toenails - An ingrown nail occurs when the nail border or
corner presses on the surrounding tissue. This condition is painful and often
results in an infection once the skin is broken (see figure 2).
Causes
- The most
common causes are improper trimming of toenails and poor hygiene.
- Trauma to the
nail plate or toe
- Improperly
fitted footwear
- Abnormally
shaped nail plate
Signs and Symptoms
- Pain
along the margin(s) of the toenail. The great toe is the most common toe
affected.
- Localized
edema
- There may be signs of infection (drainage of pus, blood, or watery discharge
tinged with blood)
Treatment
- Trim a small point off the corner of the nail to relieve the pressure. Remove
any dead skin that may have accumulated in the nail groove.
- Elevate the end of the nail to prevent further irritation of the soft tissue.
Proper trimming should correct ingrown toenail. If not…
- Surgically correct a chronic ingrown toenail at the BAS, by complete or
partial removal of toenail, under the supervision of a clinician.
- If there are signs of infection, antibiotics should be considered.
|

Substitute Figure 3: Callus* |
Corns and Calluses (see figure 3) - A callus is a thickening
of the outer layer of skin, in response to pressure or friction, that serves
as a protective mechanism to prevent skin breakdown. A corn is similar to a
callus except it involves a discrete pressure spot, typically over a bone,
whereas a callus can form anywhere.
Causes
- Tight fitting shoes, due to chronic friction and sheering pressure
- Deformed and crooked toes
- Prolonged walking on a downward slope
Signs and Symptoms
- Thickened,
dry skin over prominent bones (corn)
- Large patches of thickened,
dry skin over friction areas from walking (calluses)
- Pain on direct pressure
against the corn
- Skin breakdown and possible
infection with continued irritation
Treatment
- Debridement
of excessive buildup of skin
- Apply various pads and devices
to the toes to relieve pressure (mole skin, corn pads, etc.)
- Fix the cause (improperly
fitted boots)
- In extreme
cases, refer to a Medical Officer
|

Substitute Figure 4: Bunion* |
|

Substitute Figure 5: Plantar
Fasciitis* |
Plantar Fasciitis - Also known as heel spurs or heel
bursitis. Plantar fasciitis is one of the most common foot problems. The
plantar fascia’s main function is to anchor the plantar skin to the bone,
thus protecting the longitudinal arch of the foot. The plantar fascia is
strained from overuse, causing pain along the sole of the foot, particularly
where the fascia connects to the heel (see figure 5).
Causes
- Overuse
in the physically active or a sudden increase in the volume or intensity of
training
- Abnormal
joint mechanics
- Tightness of
the Achilles tendon
- Shoes with
poor cushioning
- Abnormal foot
anatomy
- Obesity
- Improper shoes
- Bio-mechanical problems (mal-alignment of the heel)
Signs and Symptoms
- Tenderness along the medial
fascia
- Constant pain that is worse in
the morning upon rising or after physical activity
- Tearing and pulling sensation
- Altered gait
Treatment
- Heel and arch supports (Orthotics)
|

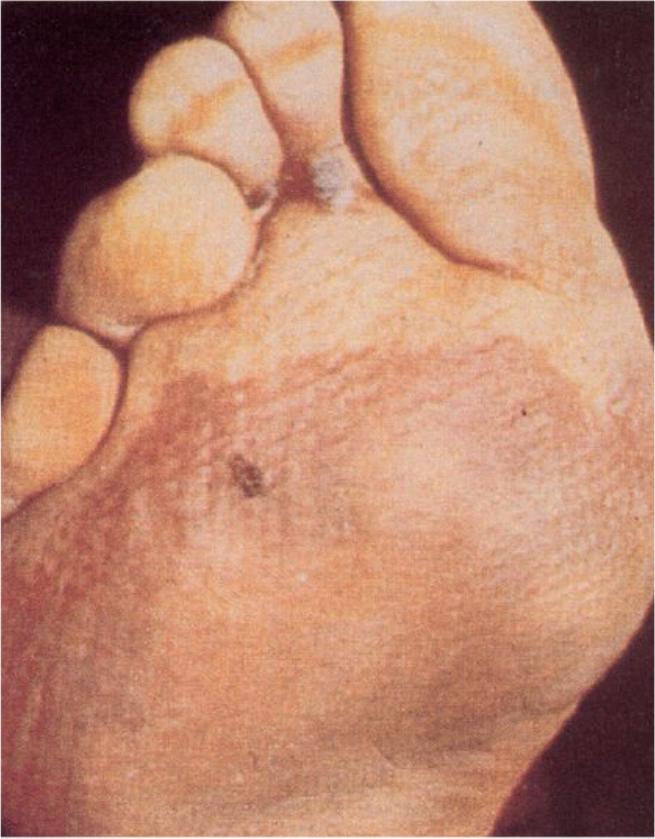
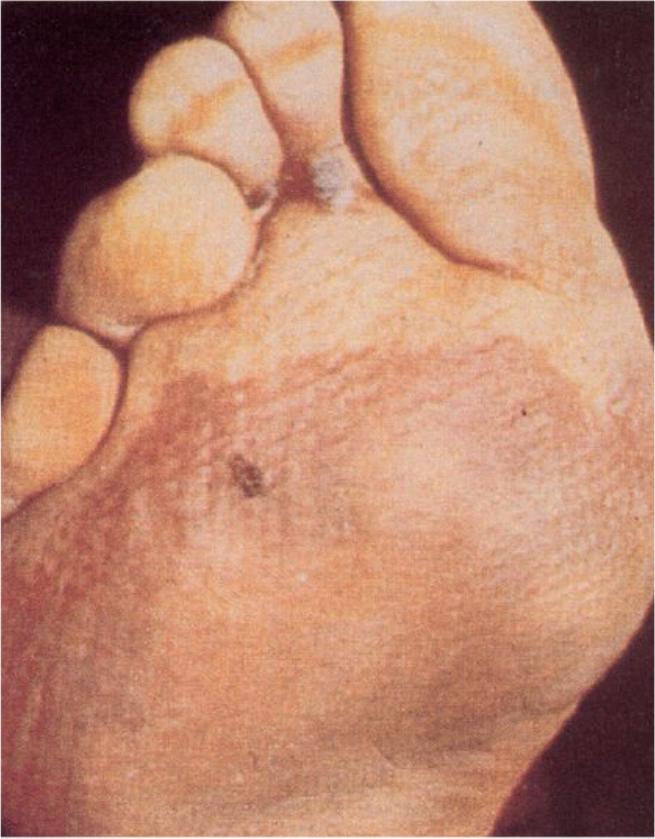
Substitute Figure 6: Plantar wart
after surgical debridement* |
Plantar Warts - Warts that are located on the sole of the
foot are called plantar warts. A plantar wart can be found as a single
lesion or grouped together. Most common areas include the ball of the foot
and heel, where increased pressure and irritation is common. Warts are
often ignored until they become painful (see figure 6).
Cause
Signs and Symptoms
Treatment
- Apply
dressing to keep paste isolated over wart. Apply donut bandage to relieve
pressure.
- Leave
paste in place for 3 days.
- Repeat
treatment in one week.
- Refer to
medical officer if no improvement.
|
Substitute Figure 7:
Immersion (Trench) Foot* |
Trench Foot/Immersion Foot - A medical
condition caused by prolonged exposure of the feet to damp and cold.
Trench Foot was given its current name after it was found frequently among
World War I troops who had been confined for long periods in trenches filled
with standing water. Immersion foot describes a more severe variant of
trench foot usually seen in downed pilots and shipwrecked Sailors (see
figure 7).
Causes
- Prolonged
exposure to wet and cold conditions or outright immersion of feet in water at
32-50° F
- Condition
can occur on hands due to damp or cold gloves
Signs and Symptoms (EARLY)
- Initially
foot is pale, mottled, numb, pulseless, and immobile
- After rewarming, severe burning pain and return of sensation
Signs and Symptoms (LATE
2-7days)
- Limb becomes hyperemic (increased amount of blood flow, skin will be warm and
red). Numbness, edema, ulceration, and gangrene may develop.
Treatment
- Treatment is supportive
- Keep
feet clean, warm, dry, and bandaged
- Gentle rewarming
- Elevate
affected extremity to reduce edema
- Consider
antibiotics if there are signs of infection
- Avoid
wearing boots
- Do not drain blisters in the
field
- Refer to Medical Officer
- CASEVAC severe cases
|

Substitute Figure 8: March Foot
(Metatarsal Stress Fracture)* |
Causes
-
Repetitive stress on a metatarsal due to malposition or abnormal foot structure
or mechanics (i.e. Flatfoot)
- Increased levels of activity, especially without proper conditioning
- Obesity
Signs and Symptoms
Treatment
- Treat as a
fracture
- RICE
- NSAIDS
- Rest for
two or three weeks until the pain is gone
- Slow
return to activity to avoid recurring injury
- Refer to
Medical Officer
3.
PREVENTIVE MEASURES
Before Marches
- Educate
troops about proper foot care and wear
- Carefully
fit new boots
- The toe box
should be roomy enough so you can wiggle your toes
- Ball of your
foot rests on the widest part of the sole
- The forefoot
should not be wider than your shoe
- Determine
the proper boot length. There should be a ˝ inch between the end of the
longest toe and the end of the boot.
- Keep feet
clean and dry
- Wear clean,
dry, un-mended, well fitting socks
- Socks should
fit snugly on the foot without excess material over toes and heel
- If a
person wants to wear two pair of socks, the outer pair should be ˝ size
larger to comfortably fit over the inner sock.
- Trim nails
straight across, and not too short. Don’t cut out or dig at corners
- Use foot
powder
- Early and
immediate attention to pain around toenails
During Rest Periods
- Lie with feet
elevated at rest points
- If time
permits, massage the feet, apply powder, change to dry socks and treat blisters.
- Relief from swelling feet can be obtained by slight loosening of the bootlaces
where they cross the arch.
After Marches
- EARLY
ATTENTION IS ESSENTIAL! As soon as any discomfort is felt, take corrective
action.
- Wash and dry feet
- Treat blisters, abrasions,
corns, and calluses if they have occurred
- If red,
swollen, or tender skin develops along the edges of the foot, the foot requires
aeration, elevation, rest, and as a rule, wider footwear
REFERENCES