FMST Student Manual - 2008 Web Edition*
|
UNITED STATES MARINE CORPS
Field Medical Training Battalion
Camp Lejeune
FMST 1419
Perform Needle Thoracentesis
TERMINAL LEARNING OBJECTIVE
1. Given
a casualty with a tension pneumothorax in a combat environment and
standard field medical equipment and supplies, perform Needle
Thoracentesis, to prevent further injury or death per the references.
(FMST-HSS-1419)
ENABLING LEARNING OBJECTIVES
1. Without
the aid of references, given a description or list, identify important
anatomical landmarks of the chest for Needle Thoracentesis, per the student
handout. (FMST-HSS-1419a)
2. Without
the aid of references, given a description or list, identify the indications
for Needle Thoracentesis, per the student handout. (FMST-HSS-1419b)
3. Without
the aid of references, given a description or list, identify the proper
equipment for performing Needle Thoracentesis, per the student handout
(FMST-HSS-1419c)
4. Without
the aid of references, given a description or list, identify the procedural
sequence for Needle Thoracentesis, per the student handout. (FMST-HSS-1419d)
5. Without
the aid of references, given a description or list, identify potential
complications of Needle Thoracentesis, per the student handout.
(FMST-HSS-1419e)
6. Without
the aid of references, given a simulated casualty and standard field medical
equipment and supplies, perform a Needle Thoracentesis, per the student
handout. (FMST-HSS-1419f)
1.
DEFINITION
AND PURPOSE
Needle thoracentesis is a procedure where a needle and
catheter are inserted through the chest wall into the pleural space.
The catheter provides a pathway for the release of accumulated pressure
within the pleural space. This procedure helps reduce pressure on the
heart, lungs and major vessels within the chest cavity that have
compromised the patient’s breathing and circulation.
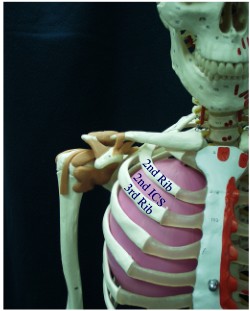
2. ANATOMICAL
LANDMARKS (See figure 1)
- Jugular Notch
- Mid-Clavicular Line
- 2nd or 3rd Intercostal Space - the 2nd
intercostal space is found by dividing the clavicle in half. From that halfway
point, palpate down one rib, and feel the first space below that rib. This is
the 2nd intercostal space (the space immediately after the clavicle
is the 1st intercostal space). The 3rd space is directly
under the 2nd.
Substitute
Figure 1. Needle Thoracentesis
Anatomical Landmarks*
3. INDICATIONS
FOR NEEDLE THORACENTESIS
Any casualty with thoracic injury is a risk for developing a tension
pneumothorax. Casualties at particular risk are those who have a
penetrating wound to the chest and those with signs of rib fracture. NOTE:
There are no significant contraindications for needle thoracentesis with
penetrating chest trauma.
4. PROCEDURAL
STEPS FOR NEEDLE THORACENTESIS
Make your Decision - based on
mechanism of injury (MOI) and a noted increase in difficulty breathing.
- Inspect - look for bilateral rise and fall of the chest
during respirations.
- Auscultate - listen to the lung fields at the mid-clavicular
and mid-axillary lines, bilaterally, if tactical situation allows (it may be
hard to hear in a combat setting).
- Palpate - feel for flail segments or crepitus.
Assemble
and Check Gear
-
Three and one quarter inch (3 ¼”) over-the-needle catheter (10 to 14 gauge)
-
Antiseptic solution (betadine or alcohol prep pads)
-
Inspect for packaging integrity
- Gloves
Prepare Patient
-
Position the patient in upright position (if possible)
-
Explain the procedure to the patient, if conscious
- Expose the anterior chest
Identify Landmarks (on the affected side)
Locate:
- Jugular
notch
-
Midclavicular line
- 2nd or 3rd
Intercostal space
Perform
the Procedure
- Cleanse the area with betadine or
alcohol
- Insert catheter into the 2nd intercostal
space just superior to the 3rd rib, at a 90-degree angle into the
skin and through the intercostal space.
- Puncture the parietal pleura - the pressure may be so
great that a rush of air may be encountered.
- Remove needle and catheter after pressure is released.
Reassess the Patient
-
IAP Chest
-
Visually inspect the neck
-
Monitor the patient’s response to the needle thoracentesis
-
Respiratory rate
-
Lung sounds
-
Skin color
- Continue to monitor the patient and reassess as necessary. Be
ready to insert a 2nd catheter if the patient does not improve.
5.
COMPLICATIONS
Hemothorax (blood within the pleural
space) - caused when the needle punctures any vessels within the chest wall.
Subcutaneous emphysema - released
air becomes trapped within the subcutaneous tissue. Feels like “rice crispies”
underneath the skin.
Air embolism - caused when the
needle enters a great vessel within the chest wall and air is accidentally
introduced into the central circulation.
Misdiagnosis - the additional trauma caused by the
needle would not be expected to significantly worsen the casualty’s condition
should they not actually have a tension pneumothorax.
|
CASUALTY ASSESSMENT AND NEEDLE
THORACENTESIS |
|
Care Under Fire
Phase: In the absence of life-threatening hemorrhage, there is no
care given to a casualty in need of a needle thoracentesis in this
phase.
Tactical Field
Care Phase: Needle thoracentesis is a skill that will be used
during the Tactical Field Care Phase in the treatment of respiratory
trauma. If a casualty has a torso injury and difficulty breathing, you
should perform a needle thoracentesis. Remember, a tension pneumothorax
can develop at any time after an injury, not just immediately after, so
continual assessment of the casualty is necessary. Complete a head to
toe assessment using DCAP-BTLS noting and treating additional injuries.
Determine if vascular access is required (see Combat Fluid Resuscitation
lesson) and give fluids if necessary. If the casualty is able to drink
fluids, they should be encouraged to do so. Consider pain medications
and give antibiotics if warranted. Reassess all care provided.
Document care given, prevent hypothermia, and CASEVAC. |
REFERENCE
Pre-Hospital Trauma Life Support, Military Edition, 6th
Ed, Chapter 10
REV: July 2008
|
FMST: |
PERFORMANCE TEST |
|
|
TASK: |
NEEDLE THORACENTESIS |
|
|
DIRECTIONS: |
Without the aid of references and given a
simulated casualty and standard field medical equipment and supplies,
perform a needle thoracentesis (FMST-HSS-1419f). |
|
|
This test evaluates your ability to
demonstrate the skills you were taught in Needle Thoracentesis. You
will be required to perform the task on a mannequin and answer oral
questions with regard to the procedure.
Safety considerations for this test
include your ability to demonstrate or verbalize universal precautions
and maintain proper “sharps” handling procedures, as you would be
required to do in any patient care situation.
There is no time limit. Should you fail
this evolution, you will be remediated and retested until you master
the skill. You will be given three opportunities to complete this
test. |
|
|
No. |
Your performance will be evaluated on
the following items: |
YES |
NO |
|
1. |
MAKE YOUR DECISION |
|
|
|
|
Visually inspect thorax for rise and
fall of chest and trauma
Auscultate thorax
Palpate topside thorax |
□
□
□ |
□
□
□ |
|
2. |
CHECK GEAR |
|
|
|
|
3.25 inch over-the-needle catheter (10-14
gauge)
Betadine and bandage packaging integrity
Gloves |
□
□
□ |
□
□
□ |
|
3. |
PREPARE PATIENT |
|
|
|
|
Place patient in an upright position, if
possible |
□ |
□ |
|
4. |
LOCATE ANATOMICAL LANDMARKS |
|
|
|
|
Identify the jugular notch
Identify the midclavicular line
Identify the 2nd or 3rd
Intercostal space (ICS) |
□
□
□ |
□
□
□ |
|
5. |
INSERT CATHETER |
|
|
|
|
Cleanse the area
Insert catheter into the 2nd or 3rd
ICS, midclavicle
Puncture the parietal pleura
Listen for rush of air |
□
□
□
□ |
□
□
□
□ |
|
6. |
CHECK TREATMENT |
|
|
|
|
Visually assess neck, i.e., trachea
midline, JVD, etc
IAP chest |
□
□ |
□
□ |
|
STUDENT’S NAME AND PLATOON |
DATE |
ATTEMPT #
|
INSTRUCTOR SIGNATURE
|
|
|
INSTRUCTOR’S COMMENTS:
|
|
| |
|
|
|
|
|
|
|
Needle Thoracentesis Review
1.
Identify the three major l andmarks
used in performing a needle thoracentesis.
2. Identify the appropriate size over-the-needle
catheter required for a needle thoracentesis.
3. Define the acronym IAP. Which step is the most
difficult to perform in a tactical setting?
4. List, in order, the six steps on the performance
checklist. |
*The FMST Student
Manual was produced by the Field Medical Training Battalion-East, Camp Lejeune,
North Carolina. This 2008 web edition has been enhanced by the Brookside
Associates, Ltd., preserving all of the original text material, while
augmenting, modifying, eliminating or replacing some of the graphics to comply with
privacy and copyright laws, and to enhance the training value. These
enhancements are marked with a red box
□
and are C. 2008, with all rights
reserved.
|
|