NAVEDTRA 13119 Standard First Aid Course - Chapter Nine - Poisoning
Poisoning
Department of the Navy
Bureau of Medicine and Surgery
Each year in the United States, there are thousands of deaths from suicide or accidental poisonings. In addition to the fatalities, approximately one million cases of nonfatal poisoning occur because of exposure to substances in everyday use such as medications, industrial chemicals, cleaning agents, and plant and insect sprays.
The Navy Occupational Safety and Health (NAVOSH) Program requires a Material Safety Data Sheet (MSDS) be readily available to all personnel working with hazardous material. MSDS's are technical bulletins produced by chemical manufacturers. They contain safety precaution information, first aid procedures, spill response, symptoms of over-exposure, and other vital safety information. The user should review MSDSs before using a hazardous material, and the MSDSs must be accessible in case of a mishap. An alternative source for the same information is the Hazardous Material User's Guide (HMUG). Emergency information is also available from the National Response Center (NRC), 1-800-424-8802 or the Chemical Treatment and Response Emergency Center (CHEMTREC) at 1-800-424-9300.
Since most poisons act rapidly, professional medical attention or assistance from a poison control center should be obtained immediately. If more than one person is present, one should obtain assistance while the other begins administering first aid. Although the symptoms of poisoning may disappear completely before professional help is obtained, the poison may have harmful or fatal after effects.
A poison can be in a solid, liquid, or gaseous state. Poisons can be ingested (swallowed), inhaled, absorbed, or injected into the body. Poisoning should be suspected whenever a sudden unexplained illness develops. The immediate area should be searched for evidence of the cause. Clues such as gases or other chemical odors may be present. Leftover food, drinking glasses, containers, or bottles may also provide clues.
Ingested Poisons
Ingested poisons are difficult to identify because there are many different kinds. Some substances are fatal in small amounts, while other substances that are safe in small amounts become fatal if large amounts are taken. Poisoning, can result from improperly stored foods, household products, or commercial substances used aboard ship. If you suspect poisoning, do not waste time trying to find the cause or the antidote, poisoning is a medical emergency.
Signs and symptoms of ingested poisoning include:
- 1. Large (dilated) or small (constricted) pupils.
- 2. Slow or abnormal breathing, chemical odors and unusual breath.
- 3. Burns or stains around the mouth.
- 4. Nausea, vomiting and diarrhea.
- 5. Excessive salivation, sweating, and tear formation.
- 6. Convulsions or seizures.
If you suspect poisoning by ingestion, do the following:
1. Monitor the airway, breathing, and circulation (ABCs). Establish and maintain an adequate open airway.
2. Position the casualty sitting and leaning slightly forward, to prevent aspiration of vomit into the lungs.
3. Obtain if possible, all containers the substance was ingested from. If the casualty vomits, obtain a sample.
4. Contact local Poison Control Center or medical personnel immediately.
5. Request medical assistance for Ingestion of poisons immediately.
A Material Safety Data Sheet (MSDS) for the material will provide more detailed first aid procedures for ingestion of the chemical.
Shellfish and Fish
Mussels, clams, oysters, and other shellfish often become contaminated with bacteria during the warm months of March to November. Numerous varieties of shellfish (Fig. 9-1) should not be eaten at all, so wherever you serve in the world, learn which local seafood is known to be safe.
Figure 9-1 - Poisonous Fish
Most fish poisoning occurs with fish that are normally considered safe to eat, but which become poisonous at different times of the year from eating poisonous algae and plankton (red tide) that appear in certain locations.
Signs and symptoms of shellfish and fish poisoning include:
- 1. Tingling and numbness of the face and mouth.
- 2. Muscular weakness.
- 3. Nausea and vomiting.
- 4. Increased salivation,: difficulty swallowing.
- 5. Respiratory failure.
First aid is directed toward evacuating the stomach contents; if the victim has not vomited, cause him or her to do so. If respiratory failure occurs, give artificial ventilation and treat for shock.
Inhaled Poisons
In the Navy, many industrial processes produce air contaminants. Workers or passersby could inhale the air contaminants and suffer adverse health affects. Routine cleaning, painting, and preservation produce toxic vapors, gases, and dusts. You can see and smell some toxic air contaminants; however, others are invisible and odorless, like cyanide gas.
Other hazardous air contaminants are by-products of certain processes that include exhaust gases from internal combustion engines; fumes or vapors from materials used in casting, molding, welding, and plating; gases associated with bacterial decomposition in closed spaces, and gases that accumulate in voids, double bottoms, empty fuel tanks, and similar spaces. Do not enter any closed compartment or poorly ventilated space until the ship's engineer, or his or her authorized representative, has tested the space and declared it safe to enter.
Signs and symptoms of inhaled poisoning include:
- 1. Excessive coughing, shortness of breath, wheezing, and a burning sensation of the nose and throat.
- 2. Pale or bluish color to skin.
- 3. Dizziness, headache, nausea, and vomiting.
- 4. Chest pain or tightness.
You may observe a variety of symptoms, from irritation to asphyxiation. Some air contaminants work slowly to damage the liver, kidneys, and central nervous system. Some materials can cause serious diseases to the same areas. If respiratory problems are not corrected, serious illness or death could occur.
If you suspect inhalation poisoning, do the following:
1. Remove the casualty to fresh air immediately. Do not enter a toxic environment without proper respiratory protection or oxygen breathing apparatus.
2. Loosen clothing around the neck and chest.
3. Monitor the airway, breathing, and circulation (ABCs). Establish and maintain adequate open airway.
4. Treat for shock.
5. Position the casualty sitting and leaning slightly forward, to prevent aspiration of vomit into the lungs.
6. Contact local Poison Control Center or medical personnel immediately.
7. Request medical assistance for inhalation poisoning, immediately.
The Material Safety Data Sheet (MSDS) for the toxic material gives the symptoms of exposure and first aid measures.
Carbon Monoxide Poisoning
Carbon monoxide, formed by the incomplete combustion of carbon, is the most common cause of poisoning by inhalation. Carbon monoxide is colorless, tasteless, and odorless. It is usually the result of faulty equipment, improper use of equipment, or poor ventillation of equipment.
Signs and symptoms of carbon monoxide poisoning include:
- 1. Throbbing headache, dizziness and nausea.
- 2. Difficulty breathing.
- 3. Irritability, loss of judgment and confusion
- 4. Chest pain, elevated pulse rate.
- 5. Normal skin, becoming pale, then bluish in color. Cherry-red appearance in high levels.
If you suspect carbon monoxide poisoning, do the following:
1. Remove the casualty to fresh air immediately. Do not enter a toxic environment without proper respiratory protection or oxygen breathing apparatus.
2. Loosen clothing around the neck and chest.
3. Monitor the airway, breathing, and circulation (ABCs). Establish and maintain an adequate open airway.
4. Treat for shock
5. Position the casualty sitting, and leaning slightly forward, to prevent aspiration of vomit into the lungs.
6. Contact local Poison Control Center or Medical immediately.
7. Request medical assistance for carbon monoxide poisoning immediately.
Absorbed Poisons
Many substances enter the body through the skin. The sap or juice of certain plants will cause skin irritation. The most common are poison ivy, oak, and sumac. The poison comes from the leaves, but it also may come from their roots and stems. The smoke from burning brush containing these plants has been known to carry the poison considerable distances. Other substances are insecticides and industrial, lawn, and garden chemicals.
Signs and symptoms of poisoning by absorption include:
- 1. Rash, itching, burning, swelling skin and blisters.
- 2. Difficulty breathing and increased pulse rate.
- 3. Fever, headache, and general body weakness.
If you suspect absorbed poisoning, do the following:
1. Remove contaminated clothing carefully, protecting yourself with gloves. do not spread the contamination.
2. Absorb liquid substances on skin, carefully brush off dry substances.
3. Flush area immediately with large quantities of fresh water, using an installed deluge shower or hose, if available. Flush area two separate times.
4. Monitor the airway, breathing, and circulation (ABCs).
5. Treat for shock.
6. Contact local Poison Control Center or medical personnelimmediately.
7. Request medical assistance for poisoning by absorption as soon as possible.
Injected Poisons
Injection of venom by stings and bites from various insects, while not normally life-threatening, can cause an acute allergic reaction that can be fatal. Any allergic reaction can develop into anaphylactic shock. Poisons also may be injected by snakes and marine animals.
Figure 9-2 - Pit Vipers Found in the U.S. and Their Bite Patterns.
Snakebite
Poisonous snakes are found throughout the world, primarily in the tropical and temperate regions. Within the United States, there are 20 species of poisonous snakes. They can be grouped into two families, the Crotalidae (rattlesnakes, copperheads, and moccasins), and the Elapidae (coral snakes).
Identification
The Crotalidae are called pit vipers because of the small, deep pits between the nostrils and the eyes (Fig. 9-2). They have two long hollow fangs, which normally are folded against the roof of the mouth, but which can be extended by a swivel mechanism when they strike. Other identifying features include thick bodies, slit-like pupils of the eyes, and flat triangular heads. Further identification is provided by examining the wound for signs of fang entry in the bite pattern shown (Fig. 9-2). Individual identifying characteristics include audible rattles on the tails of most rattlesnakes and the cotton white interior of the mouths of moccasins. These snakes are found in every state except Maine, Alaska, and Hawaii.
Figure 9-3 - Neurotoxic Snakes and Their Bite Patterns.
Coral snakes are related to the cobras, kraits, and mamba snakes in other areas of the world (Fig. 9-3). Corals, which are found in the Southeastern United States, are comparatively thin snakes with small bands of red, black, and yellow (or almost white). Other nonpoisonous snakes have the same coloring, but in the coral snake, the red band always touches the yellow band. Its short, grooved fangs must chew (bite pattern Fig. 9-3) into its victim before the poison can be introduced.
Every reasonable effort should be made to kill or positively identify the snake..
Venom
Venom is a complex mixture of enzymes, peptides, and other substances. A single injection can cause many different toxic effects in many areas of the body. Some of these effects are felt immediately while the action of other venom components may be delayed for hours or days. A poisonous bite should be considered a true medical emergency until symptoms prove otherwise.
The venom is stored in sacs in the snake's head. It is introduced into a casualty through hollow or grooved fangs. An important point to remember is that a bitten casualty has not necessarily received a dose of venom. The snake can control whether or not it will release poison and how much to inject.
Signs and Symptoms
It is essential that you be able to quickly diagnose a snakebite as being envenomated or not. Normally enough symptoms present within an hour of a poisonous snakebite to eliminate any doubt. The casualty's condition provides the best information as to the seriousness of the situation. The bite of the pit viper is extremely painful and is characterized by immediate swelling around the fang marks, usually within 5 to 10 minutes, spreading and possibly involving the whole extremity within an hour. If only minimal swelling occurs within 30 minutes, the bite will almost certainly have been from a nonpoisonous snake, or from a poisonous snake that did not inject venom. When the venom is absorbed, there is a general discoloration of the skin, followed by blisters and numbness in the affected area. Other signs that may occur are weakness, rapid pulse, nausea, shortness of breath, vomiting, shock, headache, fever, chills, and blurred vision. The eastern diamondback rattler bite is further characterized by numbness and tingling in the mouth and possibly the face and scalp. A metallic taste may be noted.
If you suspect a snakebite, do the following:
1. Move the casualty away from (the snake) danger.
2. Calm and reassure the casualty, keep them lying down, quiet, and warm. Do not give the casualty anthing to eat or drink.
3. Immobilize the casualty's affected extremity, keeping the area below the level of the heart.
4. Remove jewelry from affected area, unless the casualty objects.
5. Apply a constricting band (belt, necktie) 2 to 4 inches above the fang marks (Fig. 9-4) between the bite and the heart. It should be tight enough to stop the flow of blood in the veins but not through the arteries. Adjust the band as swelling occurs. Never place a band around a joint, the head, neck, or chest.
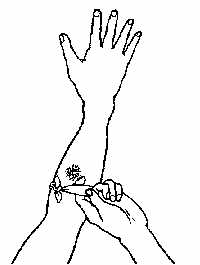
Figure 9-4. Constricting Band Properly Applied.
6. Suction the bite over the fang marks, using an extractor from a snakebite kit. Suction by mouth is recommended only as a last resort. Suction after 30 minutes is ineffective, the venom has already diffused.
7. Monitor the airway, breathing, and circulation (ABCs).
8. Treat for shock.
9. Never apply ice to afflicted area.
10. Contact nearest medical facility, if possible, so that the proper antivenom can be made available.
11. Transport the casualty (and the dead snake) as soon as possible.
Insect Stings
Insects that most commonly cause allergic reactions are honeybees, wasps, yellow jackets, hornets, and fire ants. Individuals with known sensitivities carry medication in commercially prepared kits.
Signs and symptoms of insect stings include:
- 1. Local reaction of pain, redness, itching, and swelling.
- 2. Allergic reaction of difficulty breathing or swallowing, generalized itching, redness, swelling (eyelids, lips, and tongue), hives, flushing, and abdominal cramps.
- 3. Shock may follow quickly, and death may occur.
If you suspect an insect sting, do the following:
1. Calm and reassure the casualty, keep them lying down, quiet, and warm.
2. Immobilize the casualty's affected extremity, keeping the area below the level of the heart.
3. Remove jewelry from affected area, unless the casualty objects.
4. Scrape stinger from the skin with a plastic card. Do not use tweezers.
5. Wash the area with soap and water.
6. Place a coldpack to area to reduce swelling and pain.
7. Monitor the airway, breathing, and circulation (ABCs).
8. Treat for shock.
9. Transport the casualty for professional medical treatment as soon as possible.
Spiders and Scorpions
The black widow spider is a small, glossy, jet-black spider. It has a distinctive hourglass-shaped red mark (Fig. 9-5) on the underside of its abdomen. Black widow bites are the leading cause of death from spiders in the United States.
Signs and symptoms of black widow bites include:
- 1. Pain and spasms of the back, chest, shoulders, and abdominal muscles within 30 minutes.
- 2. Nausea, vomiting, rigid abdomen.
- 3. Anxiety, fever, sweating, and rash.
If you suspect a black widow bite, do the following:
1. Apply coldpacks to affected area, do not apply ice.
2. Monitor the airway, breathing, and circulation (ABCs).
3. Treat for shock.
4. Transport the casualty (and the spider) for professional medical treatment as soon as possible.
The brown recluse spider is yellow to dark brown. It has a distinctive violin-shaped marking (Fig. 9-5) on its upper back. Brown recluse bites are non-healing and require skin grafting to repair.
Signs and symptoms of brown recluse spider bites include:
- 1. Bluish area surrounded by white, turning red (bulls-eye pattern).
- 2. Nausea, vomiting, joint pain, chills and fever within 24 hours.
- 3. Ulcer within 10 days.
If you suspect a brown recluse spider bite, do the following:
1. Monitor the airway, breathing, and circulation (ABCs).
2. Treat for shock.
3. Transport the casualty (and the spider) for professional medical treatment as soon as possible.
The scorpion is 2 to 3 inches in length with a long, narrow, segmented tail (Fig. 9-5) that ends in a venomous stinger. Stings can be fatal, most occur on the hands.
Signs and symptoms of scorpion stings include:
- 1. Pain, swelling, and discoloration at sting site.
- 2. Nausea, vomiting, seizures, restlessness, and drooling.
If you suspect a scorpion sting, do the following:
1. Apply a constricting band (belt, necktie) 2 inches above the sting. It should be tight enough to stop the flow of blood in the veins but not through the arteries. Adjust the band as swelling occurs. Never place a band around a joint, the head, neck, or chest.
2. Apply coldpacks to affected area, do not apply ice.
3. Transport the casualty for professional medical treatment as soon as possible.
Figure 9-5 - Black Widow and Brown Recluse Spiders and a Scorpion.
Ticks
The tick is 1/4 inch in length with a barbed protruding mouth part (proboscis) for attachment to the skin. They cause Lyme disease, Rocky Mountain spotted fever, and other bacterial diseases.
Signs and symptoms of Lyme disease usually occur in three stages that include:
- 1. Red rash near site, chills and fever.
- 2. Joint and muscle pain, difficulty moving, and visual problems.
- 3. Symptoms of arthritis.
Signs and symptoms of Rocky Mountain spotted fever that develop within 10 days of tick infestation include nausea, vomiting, abdominal pain, and weakness.
If the casualty has a tick, do the following:
1. Remove with tweezers, grasp as close to the skin as possible.
2. Wash the area with soap and warm water.
3. Casualty should mark the date of exposure as a reminder if medical care is needed.
Marine Life
Marine life are not normally aggressive, most injuries occur when people disturb them. Their venom causes more damage to the tissues and is destroyed by heat rather than ice.
If the casualty has a large bite (shark), do the following:
1. Remove casualty from the (danger) water.
2. Establish and maintain the airway, breathing, and circulation (ABC's).
3. Control bleeding with direct pressure, elevation, indirect pressure, or tourniquet.
4. Treat for shock.
5. Transport immediately to nearest medical treatment facility.
If the casualty has a tentacle sting (Fig. 9-6), do the following:
1. Remove, casualty from the (danger) water.
2. Gently remove tentacles and wash the area with rubbing alcohol or meat tenderizer.
3. Treat for shock.
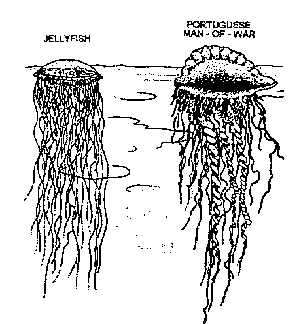
Figure 9-6 - Stinging Sea Animals.
4. Transport to nearest medical treatment facility.
If the casualty has a puncture wound (Fig. 9-7), do the following:
1. Remove casualty from the (danger) water.
2. Control bleeding with direct pressure and elevation.
3. Soak affected area for at least 30 minutes in hot water.
4. Protect the site from movement, the stinger must be removed by a physician.
5. Transport to nearest medical treatment facility.
Figure 9-7 - Stingray.
Human and Animal Bites
Human and animal bites cause abrasions, lacerations, avulsions, and punctures. Human bites that break the skin can become infected, since the mouth is contaminated with bacteria. Human bites must be treated by a physician.
Animal bites, whether domestic (dogs and cats) or wild (bats, raccoons, and rats) present the possibility of rabies in addition to tissue damage and infection. The animal should be captured and confined so it can be observed for signs of rabies. If you must take the animal's life, do not damage the head, it will be necessary to examine the brain.
If the casualty has a human or animal bite, do the following:
1. Control bleeding with direct pressure and elevation.
2. Wash the area with soap and warm water, apply a sterile dressing.
3. Transport to nearest medical treatment facility.
References
1. Karren K. J. and Hafen, B. Q. :First Responder A Skills Approach, ed. 3, Morton Publishing Company
2. NAVEDTRA 10669-C, Hospital Corpsman 3 & 2