NAVEDTRA 13119 Standard First Aid Course - Chapter Seven - Environmental Injuries
Environmental Injuries
Department of the Navy
Bureau of Medicine and Surgery
Exposure to temperature extremes, whether heat or cold, causes injury to the skin, tissues, blood vessels, vital organs, and in some cases, the entire body. Burns, heat cramps, heat exhaustion, and heat stroke are caused by exposure to heat. Hypothermia (general cooling), frostbite, and (trenchfoot)immersion foot are caused by exposure to the cold.
Burns and Scalds
Burns are caused by dry heat, and scalds are caused by moist heat. Treatment is the same for both. Contact with an electric current also causes burns, especially if the skin is dry. The seriousness of the burn can be determined by its depth, extent, and location and by the age and the health of the casualty. You must take all these factors into consideration when evaluating burns. Burns are classified (Fig. 7-1) according to their depth as first-degree, second-degree, and third-degree.
First-degree Burns
First-degree burns involve only the first (epidermal) layer of the skin. The skin is red, dry, warm, sensitive to touch, and turns (blanches) white with pressure. Pain is mild to severe, swelling (edema) may occur. Healing occurs naturally within a week.
Second-degree Burns
Second-degree burns involve the first and part of the second (dermis) layer of the skin. The skin is red, blistered, weeping, and looks (spotted) mottled. Pain is moderate to severe, swelling often occurs. Healing takes 2 - 3 weeks, with some scarring and depigmentation.
Third-degree Burns
Third-degree burns involve all layers (full thickness) of the skin, penetrating into muscle, connective tissue, and bone. The skin may vary from white and lifeless to black and charred. Pain will be absent at the burn site if all the nerve endings are destroyed and the surrounding tissue will be painful. There is considerable scarring, and skin grafting may be necessary. Third-degree burns are life threatening.
Figure 7-1, First-, Second-, and Third-degree Burns
It is important to remember that the extent (size) of the burned area (Fig. 7-2) is more important than the depth of the burn. A first-degree burn that covers a large area of the body is usually more serious than a small third-degree burn. The "rule of nines" is used to give a rough estimate of the surface area burned and aids in deciding the correct treatment. Shock can be expected in adults with burns over 15 percent or in small children with burns over 10 percent of the body surface area (BSA). In adults, burns involving more than 20 percent of the body surface area endanger life and 30 percent burns are usually fatal if adequate medical treatment is not received. The third factor in burn evaluation is the location: burns of the head, hands, feet, or genitals may require hospitalization. The causes of burns are classified as thermal (heat), chemical, electrical, or radiation.
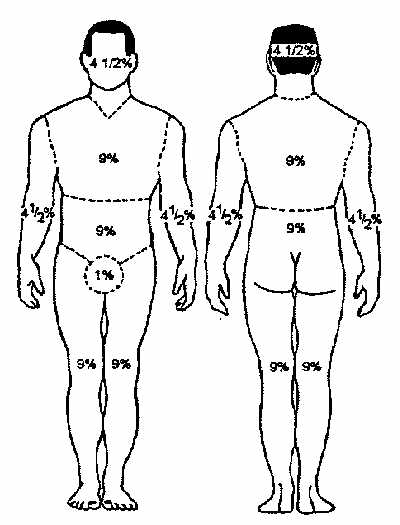
Figure 7-2-Rule of Nines
Thermal Burns
Thermal (heat) burns are caused by exposure to hot solids, liquids, gases, or fire. If the casualty has thermal burns, do the following:
1. Monitor the airway, breathing, and circulation (ABC's). Always expect breathing problems when there are burns around the face or if the casualty has been exposed to hot gases or smoke.
2. Control bleeding using direct pressure, elevation, indirect pressure, or tourniquet if indicated.
3. Remove all jewelry from the area, unless the casualty objects. Swelling may develop rapidly.
4. Apply cool water to the affected area or submerge in cool water. Do not use ice or ice water.
5. Remove clothing gently from the burned area. Do not remove clothing that is sticking to the skin.
6. Cover area with dry, sterile dressings, if possible. Cover large areas with clean, dry sheets. Do not break blisters or apply ointments of any kind.
7. Treat for shock - Keep the casualty comfortable and warm enough to maintain normal body temperature. Elevate the burned area above the heart.
8. Request medical assistance for all burns. If possible, before transport, inform medical personnel of the degree, location of the burn, and percentage of the body area affected.
Chemical Burns
When acids, alkalies, or other chemicals come in contact with the skin, they can cause injuries that are generally referred to as chemical burns. These injuries are not caused by heat but by direct chemical destruction of the tissues. The areas most often affected are the arms, legs, hands, feet, face, and eyes. Alkali burns are usually more serious than acid burns; alkalies generally penetrate deeper and burn longer.
If the casualty has chemical burns, do the following:
1. Flush area immediately with large quantities of fresh water, using an installed deluge shower or hose, if available. Avoid excessive water pressure. Continue to flush the area for at least 15 minutes while removing the clothes, including shoes, socks, and jewelry. Dry lime powder (alkali burns) creates a corrosive substance when mixed with water; keep the powder dry and remove it by brushing it from the skin. Acid burns caused by phenol (carbolic acid), should be washed with alcohol. Then wash the area with large quantities of water. If alcohol is not available, flush the area with large quantities of water. Cover chemical burns with a sterile dressing.
2. If available, follow the first aid procedures provided in the Material Safety Data Sheet (MSDS) for the chemical.
3. Flush the eyes with fresh water immediately using an installed emergency eye/face bath or hose on low pressure for at least 20 minutes. Ask casualty to remove contact lenses. Use your hands to keep the eyelids open. Never use a neutralizing agent, mineral oil, or other material in the eyes.
4. Monitor the airway, breathing, and circulation (ABCs).
5. Warning - Do not attempt to neutralize any chemical unless you are sure what it is and what substance will effectively neutralize it. Further damage may be done by a neutralizing agent that is too strong or incorrect. Do not apply creams or other materials to chemical burns.
6. Treat for shock - Keep the casualty comfortable and warm enough to maintain normal body temperature.
7. Request medical assistance for all chemical burns. If possible, before transport, notify medical personnel of the name and other pertinent information about the chemical involved, location of the burn, and percentage of the body area affected. Send the container to medical personnel with the casualty.
Electrical Burns
Electrical burns may be more serious than they first appear. The entrance and exit wounds may be small, but as electricity penetrates the skin, it burns a large area (Fig. 7-3) below the surface.
Figure 7-3. Electrical Penetration of the Skin
If the casualty has electrical burns, do the following:
1. Shut off the power. If you cannot shut off the power, remove the victim immediately. Stand on a well-insulated object, and use a dry rope, wooden pole, or other non-conductive material to either push or pull the wire away from the casualty, or the casualty away from the electrical source. Do not attempt to administer first aid or come in physical contact with an electrical shock casualty before shutting off the power. If you cannot shut off the power immediately, remove the victim from the live conductor before touching them.
2. Maintain a neutral position of the head and neck, apply a cervical collar or improvised (towel) collar. (Casualty is usually thrown).
3. Establish and maintain the airway, breathing, and circulation (ABCs).
4. Begin CPR/rescue breathing - Electrical burns are often accompanied by respiratory or cardiac arrest. If necessary start CPR (Chapter 2) immediately and continue until successful.
5. Cover burn areas with a moist, preferably sterile, dressing.
6. Treat for shock - Keep the casualty comfortable and warm enough to maintain normal body temperature.
7. Request medical assistance for all electrical injuries. If possible, before transport, inform medical personnel of the electrical source involved and the location of the entrance and exit wounds.
Sunburn
Sunburn results from prolonged exposure to the ultraviolet rays of the sun. First- and second- degree burns similar to thermal burns may develop. Treatment is essentially the same as for thermal burns. Unless a major percentage of the body is affected, the casualty will not require more than first aid attention. Commercially prepared sunburn lotions and ointments may be used. Prevention through education and the proper use of sunscreens and sunblocks is the best way to avoid this condition.
White Phosophorous Burns
A special category of burn, which may affect military personnel in a wartime or training situation, is that caused by exposure to white phosphorous (WP or Willy Peter). First aid for this type of burn is complicated by the fact that white phosphorous particles ignite upon contact with air. Superficial burns caused by simple skin contact or burning clothes should be flushed with water and treated like thermal burns. Partially embedded white phosphorous particles must be continuously flushed with water while the first aid provider removes them with whatever tools are available, such as tweezers or pliers. Do this quickly but gently. Deeply embedded particles that cannot be removed must be covered with a saltwater (saline) soaked dressing that must remain wet until the casualty receives professional medical attention. When rescuing casualties from a closed space where white phosphorous is burning, protect your lungs with a wet cloth over your nose and mouth.
Heat Exposure
Excessive heat affects the body in a variety of ways. When a person exercises in a hot environment, heat builds up inside the body. The body automatically reacts to get rid of this heat through the sweating mechanism. If the body loses large amounts of water and salt from sweating, heat cramps and heat exhaustion may develop. If the body becomes too overheated, the sweat control mechanism of the body malfunctions and shuts down. The result is heat stroke (sunstroke). Heat exposure injuries are a threat in any hot environment, especially in desert or tropical areas and in the boiler rooms of ships.
Heat Cramps
Heat cramps are muscular pains and spasms resulting from the loss of water and salt from the body. Excessive sweating may result in painful cramps of the muscles of the abdomen, legs, and arms. Heat cramps also may result from drinking ice water or other cold drinks either too quickly or in too large a quantity after exercise. Heat cramps are often an early sign of approaching heat exhaustion.
Signs and symptoms of heat cramps include:
- 1 Muscle pain and cramps.
- 2. Faintness or dizziness.
- 3. Nausea and vomiting.
- 4. Exhaustion and fatigue.
If you suspect heat cramps, do the following:
1. Move the casualty to a cool or air conditioned area.
2. If the casualty can drink, give him or her one-half glassful of cool water every 15 minutes. If the casualty vomits, stop giving water. Do not give salt tablets.
3. Gently stretch or massage the muscle to relieve the spasm.
4. Request medical assistance if the casualty has other injuries or does not respond to the above procedures.
Heat Exhaustion
Heat exhaustion is caused by the excessive loss of water and salt (sweating). It is the most common condition from exposure to hot environments (Fig. 7-4).
Figure 7-4. Symptoms of heat stroke and heat exhaustion.
Signs and symptoms of heat exhaustion include:
- 1. Pale, cool, (clammy) moist skin.
- 2. Large (dilated) pupils.
- 3. Normal or below normal temperature.
- 4. Rapid and shallow breathing.
- 5. Headache, nausea, loss of appetite.
- 6. Dizziness, weakness or fainting.
If you suspect heat exhaustion, do the following:
1. Move the casualty to a cool area, apply cold, wet compresses, and fan the casualty.
2. Treat for shock.
3. Remove the casualty's clothing, do not allow the casualty to become chilled.
4. If the casualty is conscious and can drink, give him or her one-half glassful of cool water every 15 minutes. If the casualty vomits, stop giving water. Do not give salt tablets.
5. Request medical assistance for heat exhaustion casualties as soon as possible.
Heat stroke
Heat stroke, also known as sunstroke, is a life-threatening emergency. It is not necessary to be exposed to the sun for it to develop. It is less common but more serious than heat exhaustion. The casualty experiences a breakdown of the sweating mechanism (Fig. 7-4) and is unable to eliminate excessive body heat. If the body temperature rises too high, the brain, kidneys, and liver may be permanently damaged.
Signs and symptoms of heat stroke include:
- 1. 105 degrees F (41 degrees C) or higher temperature.
- 2. Hot, wet, or dry and reddish skin.
- 3. Small (constricted) pupils.
- 4. Headache, nausea, dizziness, or weakness.
- 5. Deep and rapid breathing at first, then shallow and almost absent.
- 6. Fast and weak pulse.
If you suspect heat stroke, do the following:
1. Move the casualty immediately to a cool area, place them in a cold water bath. If this is not possible, give a sponge bath by applying wet, cold towels to the entire body. If available, place cold packs around the neck.
2. Monitor the airway, breathing, and circulation (ABCs).
3. Treat for shock.
4. Remove the casualty's clothing, do not allow the casualty to become chilled.
5. If the casualty is conscious and can drink, give him or her one-half glassful of cool water every 15 minutes. If the casualty vomits, stop giving water. Do not give salt tablets.
6. Request medical assistance for heat stroke casualties as soon as possible.
Cold Exposure
When the body is exposed to extremely cold temperatures, the blood vessels constrict and body heat is gradually lost. As the body temperature falls, tissues are easily damaged. The extent of damage depends on such factors as wind speed, temperature, type and duration of exposure, and humidity. Fatigue, smoking, drugs, alcohol, stress, dehydration, and the presence of other injuries increase the harmful effects of the cold.
General Cooling (Hypothermia)
Hypothermia, an abnormally low body temperature, is a medical emergency. It is caused by continued exposure to low or rapidly falling temperatures, cold moisture, snow, or ice. Individuals exposed to low temperatures for long periods may suffer harmful effects, even if they are protected by clothing, because cold affects the body slowly, almost without notice.
Signs and symptoms of hypothermia include:
- 1. Several stages of progressive shivering (an attempt by the body to generate heat).
- 2. Dizziness, numbness, and confusion.
- 3. Unconsciousness may follow quickly.
- 4. Signs of shock.
- 5. Extremities (arms and legs) freeze.
If you suspect hypothermia, do the following:
1. Move the casualty immediately to a warm place.
2. Monitor the airway, breathing, and circulation (ABCs).
3. Rewarm by applying external heat to both sides of the casualty. Natural body heat (skin to skin) from two rescuers (buddy warming) is the best method. Do not place heat source next to bare skin. Since the casualty is unable to generate body heat, placing him/her under a blanket or in a sleeping bag is not sufficient.
4. If the casualty is conscious and can drink, give warm liquids. Do not give hot liquids, coffee, or alcohol or allow casualty to smoke.
5. Request medical assistance for hypothermia as soon as possible.
Immersion Hypothermia
Immersion hypothermia, is the lowering of the body temperature due to prolonged immersion in cold water. It is often associated with limited motion of the extremities and water-soaked clothing. Temperatures range from just above freezing to 50 degrees F (1O degrees C).
Signs and symptoms of immersion hypothermia include:
- 1. Tingling and numbness of affected areas.
- 2. Swellina of the legs, feet or hands.
- 3. Bluish discoloration of the skin and painful blisters.
If you suspect immersion hypothermia, do the following:
1. Move the casualty immediately but gently to a warm, dry area.
2. Monitor the airway, breathing, and circulation (ABC's).
3. Remove wet clothing carefully, keep casualty warm and dry. Do not rub or massage affected area.
4. Do not rupture blisters or apply ointment to affected area.
5. If the casualty is conscious and can drink, give warm liquids. Do not give hot liquids, coffee, or alcohol or allow casualty to smoke.
6. Request medical assistance for immersion hypothermia as soon as possible.
Frostbite
Frostbite is damage to the skin due to continued exposure to severe cold. It occurs when ice crystals form in the skin or deeper tissue after exposure to a temperature of 32 degrees F (0 degrees C) or lower. The areas most commonly affected are the hands, feet, ears, nose, and cheeks. Frostbite is classified as incipient, superficial, or deep.
Incipient Frostbite (Frost Nip)
Incipient frostbite affects the tips of the ears, nose, cheeks, toes, and fingers. Casualties normally are unaware of the injury. Initially, the affected skin reddens, then becomes (blanched) white and painless. Move the casualty to a warm area. Warm the affected areas with a buddy's body heat, or by immersing in warm water. Do not rub or massage affected areas. Frostbite requires professional medical attention as soon as possible.
Superficial Frostbite
Superficial frostbite affects the surface of the skin and the tissue beneath. The skin will be firm and white, but the underlying tissue will be soft. The affected area may become blue, tingle, swell, and burn during thawing. Move the casualty to a warm area. Hands can be rewarmed by placing them under the armpit, or against the abdomen. Feet can be rewarmed by using a buddy's armpit or abdomen, other areas can be rewarmed by immersing in warm water. Do not rub or massage affected areas. Frostbite requires professional medical attention as soon as possible.
Deep Frostbite
Deep frostbite is a medical emergency that affects the entire tissue layer. The skin feels hard and is white to blue in appearance. The purpose of first aid is to protect the affected area from further damage, to thaw the affected area, and to monitor the airway, breathing, and circulation. Move the casualty to a warm area. Rewarm affected areas by immersion in water at 100 degrees F to 105 degrees F (30 degrees C to 41 degrees C). Gently dry the area with a soft towel, place cotton between the toes and fingers to avoid their sticking together. Do not rub or massage affected areas. Frostbite requires professional medical attention as soon as possible. Do not allow the affected area to be exposed to the cold.
References
1. NAVEDTRA 10669-C, Hospital Corpsman 3 & 2